COVID-19's long shadow over diabetes
24 May 2022

Written by Mark Pownall
The pandemic has changed things in so many ways, including an increased risk of diabetes in the population.
The SARS-CoV2 pandemic that the world experienced for more than 2 years is going to cast a long shadow; its length is just beginning to become apparent.
Medium-term effects of COVID-19
From the hundreds of thousands of COVID-19 papers published so far, one paper in this mountain gives us a good idea of the medium-term effects of COVID-19. Epidemiologists looked at data collected from the US Veteran Affairs (VA) administration for nearly 75,000 patients who survived 30 days after an initial COVID-19 infection and who were not admitted to hospital (mild to moderate disease). They were compared with nearly 5 million non-COVID-19 controls.
Beyond the first 30 days of an acute infection with COVID-19 and up to six months afterwards, people remain at higher risk of death and are higher users of healthcare resources, compared to controls uninfected with COVID-19.1 Post-COVID-19, people may be left with:
- respiratory symptoms
- cardiovascular disease
- malaise
- fatigue
- musculoskeletal pain
- anaemia
- and other signs and symptoms.1
They are more likely to be using painkillers (opioids and non-opioids) antidepressants, and medicines for anxiety, high blood pressure and diabetes.1
The excess risks do not affect everyone who has had a COVID-19 infection, or even a majority. But it is not trivial. For every 1,000 people infected with COVID-19, about 25 are affected by long term pulmonary symptoms.1 For dozens of other symptoms and conditions, there appears to be a higher risk.
COVID-19 and increased diabetes risk
The VA researchers published a follow-up paper in March 2022, looking specifically at diabetes and COVID-19.2
They found that those who had had COVID-19 were 40% more likely to have incident diabetes, and 85% more likely to be using therapies for reducing blood glucose levels (antihyperglycaemic agents) than controls.
The research stratified the severity of the acute COVID-19 infection (non-hospitalised, hospitalised, intensive care) and found that the more severe the acute infection, the higher the risk of later diabetes. The increased risk applied whatever the baseline risk. COVID-19 appears to increase baseline risks and accelerates the progression of diabetes among those at high risk.
Healthcare impact
Given the increasing numbers of people developing type 2 diabetes throughout the world and the gap between optimal clinical management and what happens in practice, that looks to be a huge additional burden for hard-pressed healthcare systems.
At the time of writing about 500 million people have had COVID-19, suggesting several million additional new cases, if the course of the infection described by the VA researchers plays out in the global population. The potential additional strain on health services that have been all but overwhelmed by COVID-19 is clear.
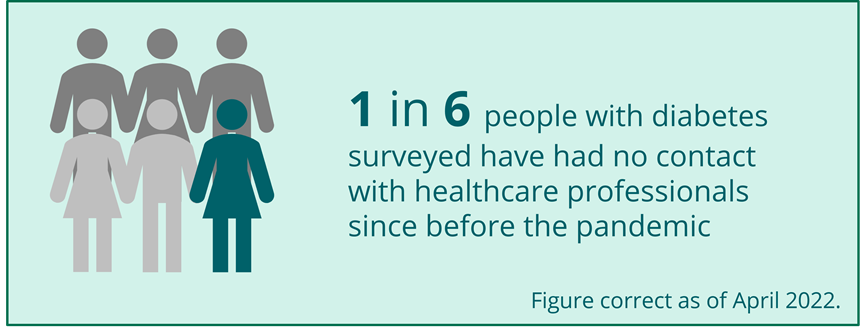
COVID-19 has already disrupted diabetes care and, according to a survey by Diabetes UK reported in The Guardian,3 people with diabetes in the UK have had, and continue to have, difficulties accessing healthcare. It was found that one in six of those surveyed have had no contact with healthcare professionals since before the pandemic. The proportion of those who have had all their recommended diabetes checks has fallen from 57% in 2019–2020 to 36% in 2020–2021. The end result is an increased risk of the complications associated with diabetes, both microvascular and macrovascular.
Next steps
At least 3 things need to happen to prevent future ill health. First it is important to re-establish the relationship between clinicians and patients, cut, or at least reduced, by the pandemic. Second there is a need for effective communication with patients to encourage them to attend their regular checks, and perhaps to look out for new COVID-19-related signs and symptoms. And then there is a need to ensure there are the resources to establish recovery services (in diabetes but also in mental health, heart disease medicine, rheumatology, etc.).
There is a long shadow attached to COVID-19, but it doesn’t need to keep us in the dark permanently.
-
Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594:259–264.
-
Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 2022;10:311–321.
-
Disruption to diabetes care during COVID-19 threatens thousands, charity warns. 20/05/2022. The Guardian. Available at: theguardian.com/society/2022/apr/20/disruption-to-diabetes-care-during-COVID-19-threatens-thousands-charity-warns. (Accessed May 2022)
Wave is a global healthcare communications agency. We combine scientific, medical and brand expertise to deliver clinically focussed programmes which are trusted by HCPs and drive better patient outcomes. To find out more, click here to read about who we are or here to read about what we do.